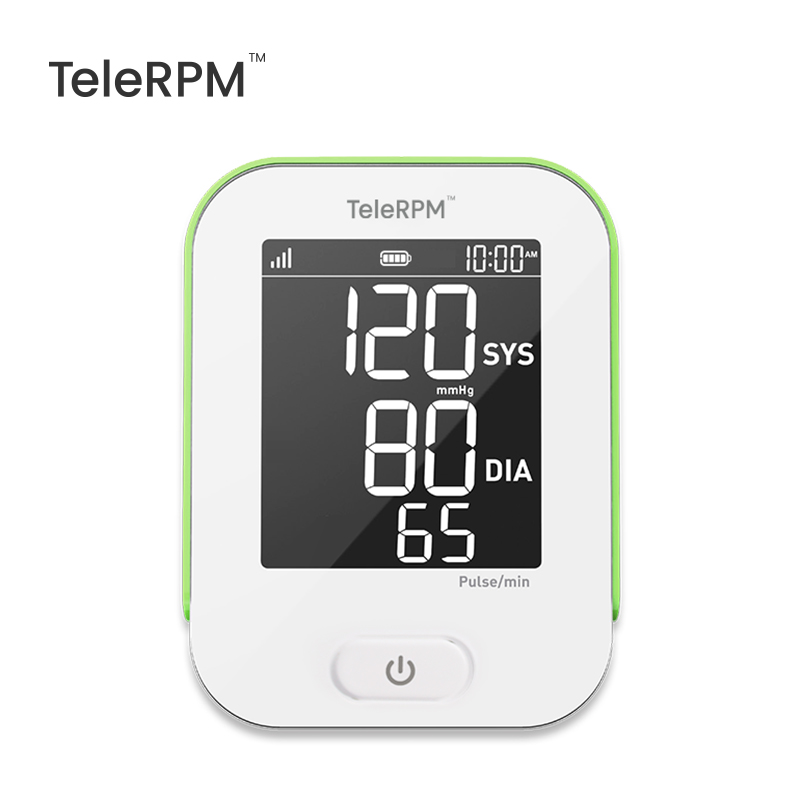
When launching a blood pressure monitor into the U.S. market, understanding and meeting Food and Drug Administration (FDA) regulatory requirements is essential. This applies to devices like Transtek’s TeleRPM BPM Gen 1 Cellular Blood Pressure Monitor, which combines standard blood pressure measurement with remote patient monitoring (RPM) connectivity.
This guide explains how blood pressure monitors are regulated by the FDA, classification and pre-market submission requirements, applicable testing standards, and post-market responsibilities.

Blood pressure monitors intended for clinical or medical use are regulated by the FDA as medical devices. These devices must balance safety, accuracy, and effectiveness before they can be legally marketed in the United States.
Automated non-invasive blood pressure monitors typically fall under:
21 CFR §870.1130 – Noninvasive Blood Pressure Measurement Systems
Class II Medical Device
Product Code: DXN
FDA lists this category for oscillometric blood pressure monitors measuring systolic and diastolic pressures.
The FDA recently issued safety communication warning against the use of unauthorized blood pressure devices that claim to measure or estimate blood pressure without FDA marketing authorization. Such devices have not been demonstrated to meet FDA safety and effectiveness requirements and may provide inaccurate readings, potentially leading to misdiagnosis or delayed medical treatment.
FDA communications emphasize that devices without proper marketing authorization cannot be considered medically reliable. The FDA explicitly states that devices without FDA marketing authorization have not been evaluated by the Agency for safety and effectiveness, and that inaccurate measurements from such devices may lead to harmful clinical decisions. Healthcare providers and procurement professionals are encouraged to use only FDA-authorized devices with verified performance and clearance status.
For most Class II blood pressure monitors intended for medical use, manufacturers must submit a 510(k) premarket notification to the FDA.This demonstrates that the new device is “substantially equivalent” in safety and performance to a legally marketed predicate device. Substantial equivalence compares intended use and technological characteristics against existing marketed monitors. Once cleared, the FDA issues a 510(k) number, and the device can be marketed in the U.S.
In a typical 510(k) application, the FDA expects:
A clear device description including intended use
Summary of predicate device and substantial equivalence
Performance testing data (lab and clinical results)
Labeling and instructions for use
Accurate statements of safety and effectiveness
The FDA’s guidance document on noninvasive blood pressure monitors outlines detailed recommendations for what information should be included in a submission, including design, operation, and testing protocols.
FDA guidance encourages manufacturers to demonstrate performance and accuracy either by comparison testing with a legally marketed predicate device, or conformance to recognized industry standards (e.g., ANSI/AAMI/ISO standards). One important standard for automated blood pressure monitors is ISO 81060-2:2018 — Non-invasive sphygmomanometers — Clinical investigation of intermittent automated measurement type, which specifies clinical performance testing protocols.
Blood pressure monitor manufacturers must provide thorough documentation of testing conditions, sample sizes, and data analysis to show the device reliably measures blood pressure within defined performance limits.
Manufacturers of blood pressure monitors must also comply with FDA’s Quality System Regulation (21 CFR Part 820), which covers design controls, risk management, process controls, and corrective and preventive actions (CAPA). The QSR sets expectations for maintaining consistent device quality throughout design, production, and post-market phases.
The FDA requires medical device labeling to be truthful and not misleading and clear about intended use, indications, and contraindications, inclusive of user instructions and safety warnings as appropriate.
Once a blood pressure monitor enters the market, manufacturers must monitor real-world use and report adverse events or safety issues to the FDA under the Medical Device Reporting (MDR) program. Systematic complaint handling enables early detection of potential issues and supports corrective actions such as updates, recalls, or labeling changes.
Products like TeleRPM BPM Gen 1 offer connectivity features for remote patient monitoring. Connected medical RPM devices must also address:
software lifecycle documentation
wireless communication performance
and data integrity, consistent with FDA digital health and cybersecurity guidance.
While many traditional blood pressure monitors simply measure pressure, remote patient monitoring devices connected versions require robust documentation of software and network interfaces to ensure data integrity and patient safety.
Meeting FDA requirements is a critical step for blood pressure monitors intended for the U.S. market. Key points include:
Understanding device classification and regulatory pathways
Preparing a thorough 510(k) submission
Demonstrating accuracy and safety through recognized standards
Maintaining quality systems and post-market vigilance
For devices like Transtek’s TeleRPM BPM Gen 1 Cellular Automatic Blood Pressure Monitor, compliance with both traditional blood pressure measurement and connected device expectations reinforces trust and acceptance in clinical and remote monitoring applications.

Most blood pressure monitors are FDA cleared through the 510(k) process, not FDA approved. “FDA approved” generally applies to Class III devices with PMA.
Most medical-grade blood pressure monitors require 510(k) clearance. Products that do not make medical or diagnostic claims may fall outside FDA medical device requirements; however, devices that claim to measure or estimate blood pressure are generally considered medical devices and require FDA authorization.
Review timelines vary, but standard 510(k) reviews often take several months, depending on submission quality and complexity.
FDA recommends validation against recognized standards such as ISO 81060-2, or equivalent clinical and bench testing demonstrating accuracy and reliability.
Yes. Connected devices must include additional documentation for software, cybersecurity, and data transmission reliability.
+86-0760-85707780