Remote Patient Monitoring (RPM) has become a cornerstone of modern healthcare, offering physicians and patients new ways to manage chronic conditions, reduce hospitalizations, and enhance patient engagement beyond traditional care settings. The RPM landscape in 2025 is characterized by both stability and change. While many of the billing and compliance rules remain consistent, new proposals from the Centers for Medicare & Medicaid Services (CMS) signal a more flexible future that could expand access and reduce administrative burdens.
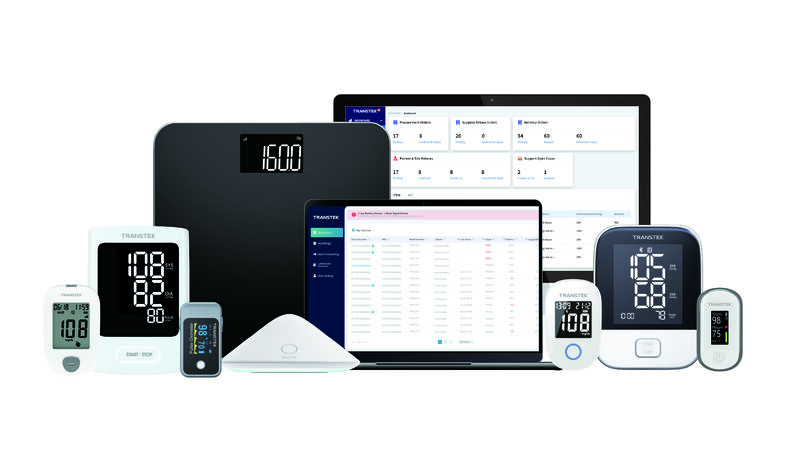
At the same time, advances in device technology, evolving patient expectations, and the growing importance of validated accuracy are reshaping how healthcare organizations implement RPM at scale. This article explores the latest updates, influencing factors, and future directions, and highlights how remote patient monitoring device manufacturers like Transtek support providers in building resilient, future-ready RPM programs.
This year reinforced familiar rules while also introducing proposals that signal more flexible pathways ahead. At the heart of current RPM billing is the 16-day rule: to bill Medicare for device supply and data transmission services (CPT code 99454), providers must document at least 16 days of patient-generated data within a 30-day period. This threshold remains unchanged in 2025, despite industry calls for greater flexibility. In addition, only one practitioner per patient per month may bill for device supply. RPM and RTM (Remote Therapeutic Monitoring) cannot be billed simultaneously for the same patient in the same 30-day period.
The CMS 2025 Physician Fee Schedule preserved these rules while signaling potential change. The most significant update is a proposal to create new device-supply codes for 2–15 days of monitoring in a 30-day period, in addition to the existing 16–30 day requirement. This proposal would allow billing for patients who do not reach the 16-day threshold, such as those onboarding late in the cycle, patients with intermittent monitoring needs, or those struggling with adherence. If finalized for 2026, this update would dismantle the “all-or-nothing” billing cliff that often penalizes programs for shortfalls in patient data.
For providers, these regulatory shifts have implications not only for compliance but also for long-term strategy. Programs that once struggled to bill for partial adherence may soon find new reimbursement opportunities, enabling them to support more patients with diverse needs. In this sense, 2025 has been both a year of stability and a year of preparation for broader change.

Adherence is the most direct driver of billable RPM months. Even the most advanced devices and protocols fail to generate value if patients do not transmit enough readings. In practice, this means that programs must implement both automated nudges and human outreach to ensure patients complete their daily or weekly measurements. Engaged patients not only improve billing consistency but also experience better health outcomes, particularly in chronic disease management.
Protocols must align with evidence-based clinical pathways. For instance, patients with hypertension require daily blood pressure monitoring, while those with heart failure benefit from daily weight tracking to detect fluid retention. COPD patients may require SpO₂ monitoring linked to symptom reports. Designing RPM around these disease-specific protocols ensures that monitoring is medically necessary, a requirement for compliance with CMS rules.
Remote patient monitoring providers must maintain detailed documentation for each enrolled patient. This includes signed consent, device shipment and activation records, day-count dashboards, and monthly interactive communication logs. Audit readiness is not optional—it is critical to sustaining an RPM program at scale and avoiding clawbacks.
Beyond direct patient care, RPM programs are also shaped by the broader telehealth policy environment. The expansion of hospital-at-home models, increasing payer acceptance, and the continued alignment of value-based care incentives have all strengthened the role of RPM as a mainstream care delivery method.
At the center of RPM program design lies a critical question: which devices will drive both clinical outcomes and financial returns? The choice of device impacts patient experience, data quality, and ultimately, reimbursement reliability.
Connectivity Reliability: Cellular-enabled devices remain the gold standard for RPM in 2025, such as cellular weight scale, cellular blood pressure monitor and cellular glucose meter. Unlike Bluetooth devices, which often require pairing with smartphones and stable Wi-Fi, cellular connectivity for remote monitoring is out-of-the-box. This reduces onboarding friction and ensures more consistent data transmission, especially for older adults or patients in rural areas with limited broadband access.
Clinical Validation and Regulatory Status: Devices must be FDA-cleared and clinically validated for accuracy. This is not only important for provider trust but also for payer confidence.
Ease of Use for Patients: Low-friction design directly impacts adherence. Devices that work immediately upon arrival, without technical setup, significantly reduce drop-off rates.
Fleet Management Capabilities: For health systems managing hundreds or thousands of devices, logistics matter. Remote diagnostics, lost device workflows, and efficient replacement processes all reduce operational overhead and protect ROI.
The rapid pace of regulatory and technological change in RPM demands a future-proof strategy. Transtek supports providers by aligning its RPM devices and infrastructure with emerging requirements:
Clinical Accuracy and Trust: Transtek monitors carry the validation that physicians and payers demand, reducing compliance risks and fostering adoption.
Seamless Patient Experience: Devices that arrive ready to use remove barriers for older adults and underserved populations, ensuring broader program reach.
Scalability for Providers: Transtek’s RPM solutions integrate with provider workflows, supporting remote diagnostics and streamlined replacements.
By focusing on accuracy, usability, and adaptability, Transtek empowers providers to scale RPM programs that are resilient to future policy shifts and capable of supporting broader healthcare transformation.
Looking beyond 2025, RPM is poised to expand as healthcare systems double down on decentralization, hospital-at-home models, and chronic disease management. Several trends are shaping the next phase:
Billing Flexibility: The likely adoption of 2–15-day device supply codes will bring RPM within reach for more patient populations, from post-surgical recovery monitoring to intermittent rehab protocols.
Integration with Broader Telehealth Ecosystems: RPM will increasingly connect with other digital health tools, including electronic health records, predictive analytics, and AI-driven care coordination.
Population Health and Value-Based Care Alignment: As more payers and providers adopt value-based models, RPM will serve as a critical data source for risk adjustment, care coordination, and outcome tracking.
Transtek’s investment in cellular-enabled, validated devices positions it as a reliable partner for providers navigating this evolving landscape. By combining accuracy, compliance readiness, and patient-friendly design, Transtek helps ensure that RPM continues to deliver value, not only for billing but also for better health outcomes.
+86-0760-85707780